Stanford University
Click Here For Further Information On Current EB Studies
Manufacturing and Incorporating Genetically-Corrected Skin and Esophagus Replacement Tissue
Click Here For Further Information On Krystal Biotech’s Clinical Trials
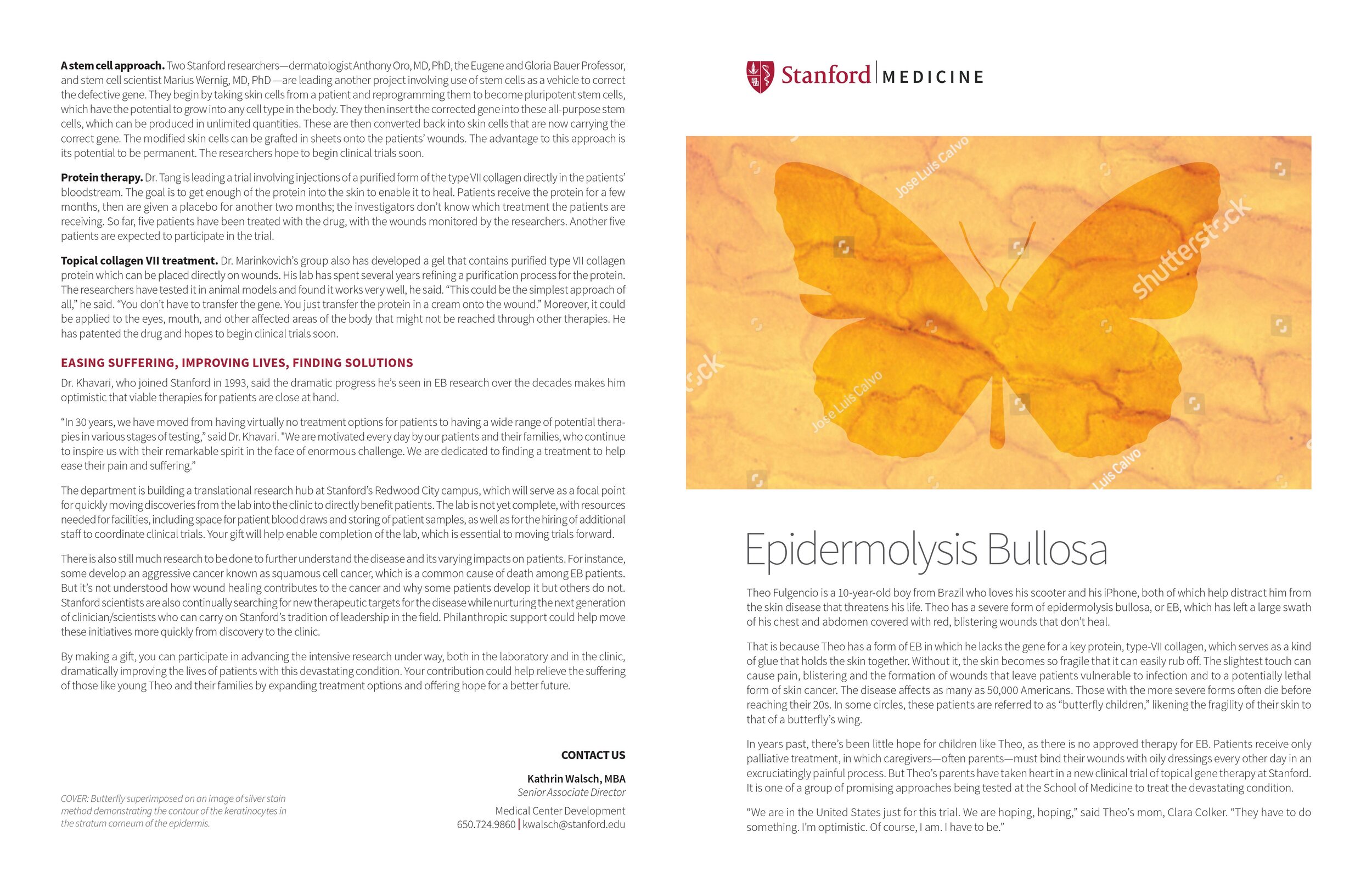
Paul Martinez was a participant in Stanford’s clinical trial for epidermolysis bullosa patients. Max Aguilera-Hellweg
Grafting sheets of a patient’s genetically corrected skin onto open wounds caused by the blistering skin disease epidermolysis bullosa appears to be well-tolerated and improves wound healing, according to a phase-1 clinical trial conducted by researchers at the Stanford University School of Medicine.
The results mark the first time that skin-based gene therapy has been demonstrated to be safe and effective in patients.
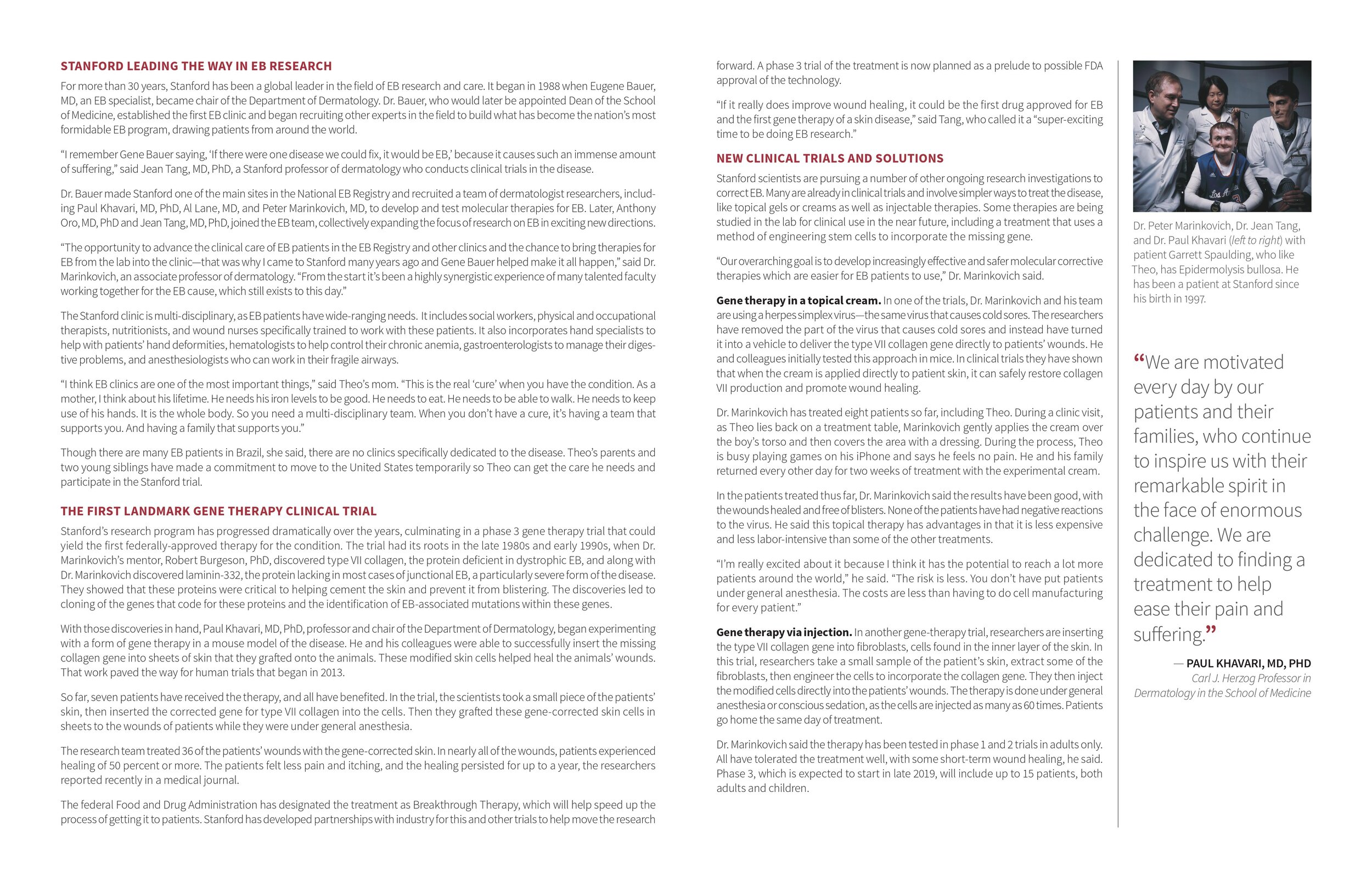
The findings were published Nov. 1 in JAMA. Associate professors of dermatology Peter Marinkovich, MD, and Jean Tang, MD, PhD, share senior authorship of the study. Senior scientist Zurab Siprashvili, PhD, is the lead author.
For the study, four adult patients with recessive dystrophic epidermolysis bullosa, an excruciatingly painful genetic skin disease, received the skin grafts.
“Our phase-1 trial shows the treatment appears safe, and we were fortunate to see some good clinical outcomes,” said Tang. “In some cases, wounds that had not healed for five years were successfully healed with the gene therapy. This is a huge improvement in the quality of life for these people.”
People with epidermolysis bullosa lack the ability to properly produce a protein called type-7 collagen that is needed to anchor the upper and lower layers of the skin together. As a result, the layers slide across one another upon the slightest friction, creating blisters and large open wounds. The most severe cases are fatal in infancy. Other patients with recessive dystrophic EB can live into their teens or early adulthood with supportive care. Often these patients die from squamous cell carcinoma that develops as a result of constant inflammation in response to ongoing wounding.
The Stanford researchers showed that it was possible to restore functional type-7 collagen protein expression in patient skin grafts to stop blistering and allow wounds to heal. They also found that the protein continued to be expressed and that wound healing was improved during a year of follow up.
The researchers seek to build upon these promising early results in a new trial that will include patients ages 13 and older.
Martinez displays an experimental skin graft on his left hand. EB patients often develop “mitten hand” caused the skin fuses after repeated rounds of wounding and scarring on the fingers and palms. Max Aguilera-Hellweg
“Moving into the pediatric population may allow us to intervene before serious chronic wounds and scars appear,” said Marinkovich, who directs the Stanford Blistering Disease Clinic. Repeated rounds of wounding and scarring on the fingers and palms, for example, often lead to fusion of the skin and the formation of what’s known as a “mitten hand.”
Siprashvili used a virus to deliver a corrected version of the type-7 collagen gene into batches of each patient’s skin cells that had been harvested and grown in the laboratory. He coaxed these genetically corrected cells to form sheets of skin about the size of an iPhone 5. The sheets were then surgically grafted onto the patient’s chronic or new wounds in six locations.
The researchers tracked the status of the grafts at one-, three- and six-month intervals for at least a year, checking to see if they stayed in place and caused wound closure. They also looked for any evidence of an immune reaction to the grafts, and whether the grafts continued to make the corrected type-7 collagen protein.
All 24 grafts were well-tolerated, the researchers found. Furthermore, they could detect expression of the type-7 collagen protein in the correct location of the skin in nine out of 10 tissue biopsies at three months. After 12 months, they were able to detect the collagen protein in five out of 12 biopsies.
Similar results were seen with wound healing. After three months, 21 of the 24 grafts were intact. This number dropped to 12 out of 24 after one year. Peter Marinkovich; “Even a small improvement in wound healing is a huge benefit to the overall health of these patients,” said Tang. “For example, it may reduce the likelihood of developing squamous cell carcinoma that often kills these patients in young adulthood.”
Coupling grafts with hand surgery to break up scarred, fused tissue could help patients maintain the use of their hands, Marinkovich said.
Tang, Marinkovich and their colleagues will continue to monitor the patients in the phase-1 trial throughout their lifetimes to assess any long-term effects of the grafts.
The completion of the phase-1 trial and the potential to improve upon these outcomes is due to a concerted, long-term effort at Stanford to find ways to help young patients with this devastating disease.
The researchers are now starting a phase-2 clinical trial and are looking for new patients. For more information, send an email to tangy@stanford.edu or mpm@stanford.edu.
Even a small improvement in wound healing is a huge benefit to the overall health of these patients.
“This trial represents the culmination of two decades of dedicated clinical and basic science research at Stanford that began with the arrival of the former dean of the School of Medicine, Eugene Bauer, who set up the multidisciplinary EB Center at Stanford,” said Tang. “We have been working for a long time to get to this potential therapy into patients. We had to discover the genes and proteins involved and the responsible mutations. We then had to learn to deliver the corrected gene and grow those cells into sheets suitable for grafting.”
“We could not have reached this point without the support of the EB patients and their families,” said Marinkovich. “Since the time of my research training in the laboratory of Robert Burgeson, PhD, who discovered type-7 collagen, I’ve been deeply motivated to contribute to the EB community, and it is very satisfying to be able to finally see this molecular therapy come to fruition.”
The work is an example of Stanford Medicine’s focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Other Stanford co-authors are research assistant Ngon Nguyen; former research associates Emily Gorell and Kylie Loutit; clinical assistant professor of dermatology Phuong Khuu, MD; clinical assistant professor of anesthesiology Louise Furukawa, MD; professor of surgery Peter Lorenz, MD; former instructor of dermatology Thomas Leung, MD, PhD; clinical associate professor of dermatology and of pathology Kerri Rieger, MD, PhD; professor of dermatology Paul Khavari, MD, PhD; and professor emeritus of dermatology and of pediatrics Alfred Lane, MD.
The research was supported by the National Institutes of Health (grant R01AR055914), the Epidermolysis Bullosa Medical Research Foundation and the Epidermolysis Bullosa Research Partnership.
Stanford’s Department of Dermatology also supported the work.
2015
HTTP://STANMED.STANFORD.EDU/2015SUMMER/THE-BUTTERFLY-EFFECT.HTML
Stanford Dermatology gratefully acknowledges the support of the EBMRF who has helped us in our EB research studies in several ways. For over twenty years, Stanford Dermatology has had a major clinical and research focus on EB, especially recessive dystrophic epidermolysis bullosa (RDEB). RDEB patients suffer from skin blistering which is caused by lack of type VII collagen, a protein which acts as a glue to hold the two layers of the skin together. This deficiency is caused by mutations of the type VII collagen gene. The key to therapy of RDEB is to restore normal type VII collagen back into the skin again, and Stanford has taken several approaches towards this goal.
Gene Therapy
One method to restore type VII collagen is to replace the faulty type VII collagen genes in the patient skin cells with a correct copy. We are currently doing this through a Food and Drug Administration (FDA) approved phase I clinical trial to study type VII collagen gene transfer for recessive dystrophic epidermolysis bullosa (RDEB). In this trial, we culture RDEB skin cells from patient biopsies and transfer the normal type VII collagen gene back into the patient skin cells using a gene transfer tool called a retrovirus. Production of the retrovirus takes place at special facilities that operate at the Good Manufacturing Practice (GMP) clinical regulatory standard.
Once the type VII collagen gene is transferred, the corrected skin cells are arranged into a sheet that is placed on patient wounds, then sutured and bandaged in place. Production of the RDEB skin cell sheets and transfer of the type VII collagen gene takes place at a culture facility at Stanford, prepared especially for EB patient research and the grafting takes place at the Lucille Packard Children’s Hospital at Stanford by trained surgeons and anesthesiologists who have experience with EB patient care. Patients are grafted with six of these sheets, each of which is approximately the size of a playing card, over chronic wounded or scarred areas.
So far four RDEB patients have been grafted with these gene corrected sheets using the patients own skin cells. We have been monitoring the clinical appearance of the grafts, and performing biopsies to look by light and electron microscopy to verify correct localization of type VII collagen protein into anchoring fibrils, the basement membrane structures which normally contain this protein. We are performing these studies in association with a National Institute of Health (NIH) organized committee which oversees our activities and ensures patient safety. These studies are currently in progress and we expect to submit our results to peer reviewed publication later this year.
We expect this therapy will achieve long term remission from blisters, scarring and perhaps inhibit future skin cancer development and expand the quality of life for adults and children with RDEB. We are currently looking to graft one more patient as part of this trial. If you are someone you know might be interested, please refer to the following link.
http://dermatology.stanford.edu/gsdc/eb_clinic/trials/eb-gene.html
Protein Therapy for EB
As an alternative to transferring the type VII collagen gene into RDEB patient skin cells, we are also exploring ways to inject type VII collagen protein into RDEB skin. Type I collagen has been injected into the skin with standard syringes and this is a well established practice in Dermatology for treating wrinkles. However conventional needles are inefficient in transferring type VII collagen, which needs to be delivered in a very precise area in the basement membrane of the skin. With this in mind, we chose to optimize the delivery of type VII collagen using biodegradeable microneedles. The benefits of these devices is that the depth and spacing of the needles, as well as the amount of protein they can contain can all be adjusted to optimize type VII collagen delivery to its precise location in the skin. Then when placed in the skin, they are dissolved by human serum, and then the needles slowly release type VII collagen. These needles are almost painless, and due to their precise delivery of type VII collagen, we feel these are the optimal delivery devices for epidermolysis bullosa patient use. We have shown that these microneedles can be steriled and freeze dried while preserving the function of type VII collagen. Ultimately we envision that the microneedle patches can be applied like wound dressings to patient skin, in outpatient or even home settings. Our hope is that this type of therapy can have a wide applicability.
We have developed stable cell lines which produce large amounts of type VII collagen suitable for industrial production using large volume cell reactors. We have specially engineered our cells so that the collagen they produce is as stable and long lasting as possible. We have recently entered into a formal collaboration with the leading microneedle manufacturer Corium. Corium is currently working at incorporating our type VII collagen into their microneedle patches.
We have finalized the purification protocol for type VII collagen protein production and reached a degree of purity which we believe is sufficient to support initial clinical trials. We hope to be able to deliver type VII collagen to wound edges so that the wounds that do not heal may now heal. We also hope to deliver type VII collagen to non-wounded skin in order to make it stronger and more resistant to trauma. We plan to initiate a pre-IND conference with the FDA by fall 2015 to lay the ground work for our clinical trial studies.
Stem Cell Therapy for EB
In addition to protein and gene therapy, we are also working on stem cell therapy for recessive dystrophic EB. The discovery of induced pluripotent stem (IPS) cells and the ability to edit the DNA mutations of these cells directly bring the possibility to provide definitive corrective genetic therapy of EB patients own skin cells. Using this IPS approach, we corrected RDEB patient skin cell gene mutations, and assembled them into sheets for grafting.
We showed that these IPS cells secreted wild-type type VII collagen, and produced normal appearing skin in basic laboratory studies. One of the advantages of using IPS cells is that it enables us to screen the cells for potential cancer predisposing gene mutations, and to select IPS cell clones which do not have these mutations. These studies lay the foundation for future clinical studies for correction of RDEB patient skin and, with additional preclinical work, we anticipate that this trial will be open for enrollment within several years.